A new Regulatory Framework for Aged Care: considerations for existing providers
Written by Lauranne Beernaert, Sector Support Coordinator
The Aged Care reforms will change the way Aged Care is assessed, funded and regulated. Together with the new Aged Care Act, the new Support at Home and its modernised regulatory framework will aim to strengthen and enhance the protection and rights of older Australians.
The below figure illustrates how the new regulatory design approach is intended to be person centered, and how protecting senior Australians will be the responsibility of all stakeholders:
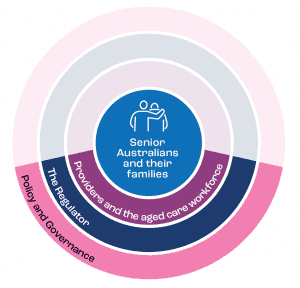
Fig 1. A person-centered approach (extracted from the Concept Design)
Key changes from the old to new regulation framework
- Move from a provider centered framework to a human rights, person-centered approach
- Move from one size fits all approach to a differentiated, risk proportionate approach
- Better use of data and resources to understand and anticipate risks across the sector/providers
- Go beyond compliance and a Pass/Fail system towards a culture of continuous improvement
- Streamlined regulation of providers working across other sectors, such as the NDIS and veteran’s care
- Aimed to be flexible and fit for purpose for future generations, regardless of funding or policy.
More information about the new proposed regulatory framework Concept Design, and a simplified English version can be accessed here.
Implications for providers
This proposed framework raises important questions for all existing providers. It invites providers to reflect on who they are today (what service they currently deliver), and who they want to be by July 2023 (which services do they want to deliver)? Do you have the capability to transform your organisation for the new Support at Home program, or do you need to consider investing in resources to help you move your business through the reforms?
A. Which service type, which level of risk?
There will be differentiated regulation arrangements based on market segmentation, location, performance and type of services delivered. For example, a gardening service will present significantly less risks to the older Australian accessing it than a personal care service, and hence will be subjected to lower requirements.
- While we are yet to receive any details about the categories/levels of the new framework, this presents the opportunity for providers to reflect about their current service offer and the anticipated category of risk they will be subjected to, and whether they want to pursue it, or change it.
- Data and intelligence relevant to the registration categories and risk will inform providers/workforce about specific education options. This means that there will be higher education/training needs and requirements for staff who deliver services included in higher risk categories.
- Market entry, including registration obligations, approval and agreement based on risk category. For example, there will be lower barriers to entry for providers with lower risk services. This means that we will see new entrants in this market. How competitive is your organisation compared to others, what is your added value?
- Rules and Standards: specific to the service type and registration category.
- Monitoring, assessment and reporting will be risk-based. They will also be graduated to drive improved quality and safety.
- Compliance and enforcement: will be flexible and modern tools will respond to emerging risks and will oversee the Sector.
Additionally, responding to these questions about the risks will have significant impacts on the organisational level. For example, think about governance requirements if you are providing high level care services, and your staffing case mix. Do you need to think about hiring a Clinical Governance Director and/or and a clinical team?
B. Government’s contribution to Aged Care, and a potential gap
The Government has committed to contribute to the cost of Aged Care. Supported by the Independent Hospital and Aged Care Pricing Authority, a price schedule would determine the price of each service type in the Service List. The set price would include the government subsidy which would reflect the cost of delivering the service, including administrative overheads. More details in the Support at Home Program Overview (page 7).
This means that there may be a gap between the Government’s subsidy and your actual service cost. Who will cover the ‘gap’? Providers, consumers or both? This re-emphasises the need to know the full cost of service delivery, and what this means in the future Aged Care environment. If there is a gap, how can you fund it or reduce it? Will your current Aged Care consumers be willing to cover the difference? Do you need to partner with a different organisation to share operational infrastructure (e.g. motor vehicle, corporate services, etc) to reduce costs? More ideas about how to collaborate within the Sector are available in our Learning Library.
What’s next?
- Get involved in consultations regarding Support at Home and the new regulatory framework. This Consultation Calendar outlines key dates and activities.
- Decide about your organisation’s future service provision and understand how a risk-proportionate regulation will apply to you at all levels (organisational, but also your position in the future Aged Care market). This might mean changing your service offer/location/etc.
- Participate in conversations and/or training that further discuss the strategic and operational implications of the new Support at Home program, such as our Managing System Changes – Round Table for CEOs to be held on 13 April 2022.
- If you decide to transition to the Support at Home program, CHSP and HCP providers will need to register as providers for the purpose of the new Aged Care Act between October 2022 and June 2023.
- Align business processes to the new payment arrangements.
- Prepare for the introduction of new regulatory reporting requirements applicable to your specific organisation/service.