Best Practice in Care February Article – Wellness and Reablement

Wellness and reablement is a hot topic in home and community care, but how can providers and frontline workers do it well? Below our aged care expert Glen Sorensen discusses how to successfully implement a quality wellness and reablement approach by partnering with consumers.
How do you define wellness and reablement?
Although wellness and reablement are two words that are often used interchangeably, in fact they describe two different aspects of an overall approach to support provision.
Wellness is about two key things. Wellness focuses first and foremost on a person’s strengths and abilities, using these as a basis for the development of an individualised support plan. Secondly, wellness is about strengthening and supporting maximum independence in daily living, whatever independence means to the person. The wellness approach is ongoing throughout the person’s support journey.
Reablement is a subset of wellness. The major difference is that it is a time-limited process that aims to address a person’s specific barriers to independence and support them to getting back to doing things for themselves. Reablement support might only be needed for one or two occasions or for short periods, usually up to three months. In reablement, it is very important to know the desired endpoint and to have a timeframe for achieving it.
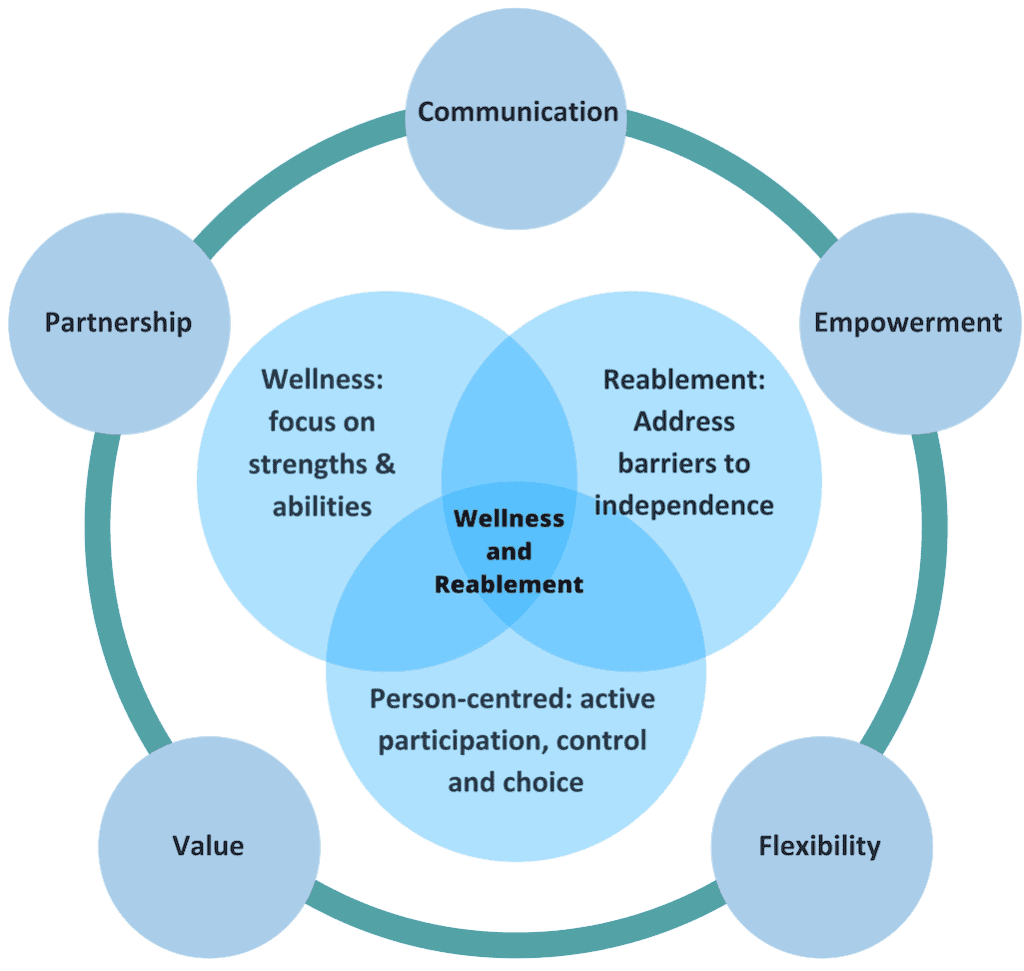
Figure 1. Wellness and Reablement Model created by Ilsa Bird
How does wellness and reablement reflect the principles of person-centred care?
Wellness and reablement approaches sit within an overarching model of person-centred practice. Person centred practice assumes that the person wants to:
- live in a preferred, appropriate environment
- be in charge rather than be controlled by others
- have the key role in decisions affecting them
- stay connected to people, communities and activities that are important to them.
As the term implies, person centredness places the person as an active participant at the centre of decision-making on issues affecting their everyday life. Supports and services are built around the person rather than the other way around. In person centred practice, the person is encouraged to take maximum control of support provision, exercising maximum choice in what, how, when and by whom support is delivered.
In essence, reablement is a subset of the wellness approach which is, in itself, a subset of person-centred practice.
What are the benefits of a wellness and reablement approach for consumers?
Almost everyone wants to stay living in their own home as independently as possible for as long as possible. Under the wellness and reablement approach, consumers remain active and engaged in daily life; continue to do whatever they can to support themselves; and take the lead role in decisions affecting them. This can have spin-off benefits for physical strength, flexibility, balance, socialisation and emotional and mental health. Having a sense of control and exercising personal power enhances self-esteem and adds to a sense of purpose to life. All of these benefits are important components of overall wellbeing.
What are the benefits of a wellness and reablement approach for providers?
The wellness and reablement approach also has numerous benefits for providers. Under this approach, consumers are less likely to become dependent on providers. Resources can go further as more consumers can be supported when providers are not assisting consumers in activities of daily living that they really could do themselves. This means that providers can concentrate on providing support in areas of real need. Frontline workers, both paid support workers and volunteers find greater job satisfaction when they see consumers playing an active part in maintaining their own independence and feel that they are contributing to this in meaningful ways.
How can service providers implement wellness and reablement strategies for people living with dementia?
When applied to people living with dementia, the focus of the wellness approach is usually on preserving functionality and wellbeing. Strategies may focus on reducing social isolation, building and supporting routine, supporting the carer and in practical strategies aimed at supporting the person and their carer to live well with dementia.
In these situations, support under a wellness and reablement approach can be about:
- establishing the right physical environment for enabling by making adjustments in the home (e.g. clutter-free circulation spaces, labelling cupboards, keeping daily used items in sight, ensuring colour contrasts between seating and the floor)
- facilitating and encouraging life participation opportunities (e.g. establishing routines, involvement in meaningful activities rather than time fillers, arts activities and hobbies that calm)
- introducing appropriate aids, equipment and assistive technology.
What are some of the barriers that exist for providers in developing wellness and reablement approaches and how might these be overcome?
One common barrier is a belief in entitlement. Consumers and their families can argue that they are entitled to support services just because they have reached a certain age, have paid their taxes or served their community or country in some way. These, in themselves, are insufficient grounds for eligibility for home support and home care provision. Providers need to be clear and firm about this from first contact.
Another common challenge is consumers and their families devolving responsibility for daily tasks because they believe this is the role of providers. Why should I do this when you are paid to do this? There are two key ways to address these assertions. First, the work of providers is subsidised, not fully funded by government. They are designed to supplement the consumer’s ability to complete ADLs not take them over. CHSP and HCP are paid supports that should not replace informal supports such as family. Secondly, it can be helpful to ask questions that encourage consumers to think for themselves about the endpoint if they aren’t committed to staying as active and involved in their lives as possible. Is this a future they would want for themselves?
How can service providers engage with consumers to develop a wellness and reablement approach that is person centred?
Engagement starts at the first point of contact. Providers should ensure that intake and assessment staff understand and can explain the approach in plain language. This can mean substituting words like ‘wellbeing’ and ‘short-term support’ for less commonly used words like ‘wellness’ and ‘reablement’. It can be extremely useful to have information sheets or information on the website and social media to back-up verbal information.
Some other practical ideas are:
- asking consumers what independence means to them and what they may need to do differently or to change to stay living as independently as they can
- asking permission whenever there is the option to do so (e.g. Is it all right if I sit here, start with this task, etc). This reinforces that the consumer has control
- ensure that the consumer is included and consulted on all decisions affecting their support provision
- noticing and applauding change and progress
- working ‘with’ rather than ‘for’ by recognising strengths and abilities and not taking over ADL tasks and sub-tasks that the consumer is able and willing to do.
How can providers engage with consumers to evaluate wellness and reablement strategies?
This is one of the big-ticket items for 2019. Although the Commonwealth wants measurable outcomes for wellness and reablement strategies, it has provided little guidance to date on how to do this effectively.
There are three major ways to engage with consumers to evaluate outcomes within a wellness and reablement approach.
- Goal attainment scaling (GAS) is a technique that gauges progress against goals. GAS not only assesses whether the goal has been reached but to what extent this has happened. The effectiveness of the technique does rely on the quality of the goal. For more information, read here about how the Younger Onset Dementia Key Worker Service collaboratively evaluated their services using GAS.
- Administration of validated and reliable tools that have been proven to measure aspects of functionality and wellbeing. Information about tools designed for disability and aged care settings can be found on the Australian Centre on Quality of Life website.
- Consumer testimony via surveys, personal interviews and focus groups. It can be helpful to have separate processes for collecting information on the consumer’s experience with the provider’s services (e.g. opinion of staff) from the outcomes they have achieved (more strength, better relationships, etc). However, the usefulness of information does depend on the quality and wording of questions asked.
How does wellness and reablement change or impact frontline service delivery? What is the responsibility of frontline care workers?
Frontline workers are arguably the most important factor in successful delivery of support under the wellness and reablement approach. Smart providers invest wisely in training and ongoing support of frontline staff. Getting support work right within a wellness and reablement approach requires:
- comprehensive briefings that include information about what the consumer is trying to achieve and the support worker role in assisting them to get or stay where they want to be
- showing interest in the person, their life, environment and achievements
- being flexible to respond to consumer preferences within the boundaries of the support plan
- not taking over tasks that the consumer can or wants to be able to do
- taking every opportunity to work alongside the consumer as a partner
- good systems for reporting back on achievements and reflecting with supervisors and co-workers on their wellness and reablement practice.
If you would like to know more, Glen will be delivering a workshop on behalf of Your Side titled ‘Engaging Consumers in Wellness and Reablement Approaches’ on February 20. To register, click here.
This year our article series ‘Best Practice in Care’ will examine what quality looks like in the sector and offer practical advice for operational and frontline procedure. The series will cover topics such as palliative care, reducing social isolation, elder abuse prevention, becoming a dementia friendly organisation and supporting caregivers and families.
The next article in our series will discuss the implementation of the new standards and engaging with consumers. To receive this article, sign up to our e-Bulletin here.
Download a printable version of this article here.
About the Author
Glen Sorensen has over 30 years continuous experience in community aged care as a service provider, academic, government officer and consultant. He founded his consultancy practice, Age Communications in 1988. In the past seven years, he has increasingly specialised in the area of wellness and reablement, designing and delivering training on a range of related topics, developing a range of resources for government, sector support, CHSP and HCP providers and the private sector and presenting at consumer forums across NSW.
